- Home
- Employers
-
Members
-
Member Resources for Funding Advantage & Individual Advantage
>
- Explanation of Benefits for Funding Advantage Members
- Member FAQs
- Member-Hybrid >
- Member-Traditional >
- Member-Essentials >
- Member-PPO >
- Member-Cost Saver >
- Member-Minimum Essential Coverage >
- Member - Community Health Plan >
- Member-H&H PLan >
- Member-Vault PPO Resources >
- Member-Vault RBP >
- Member-Fundamental Care
- Member-Fundamental Care Value Plan
- Member Resources for Individual Advantage
- Benefit Extras >
- Self-Service Login >
- Find A Provider
- Prescription Benefits
- Member Download Forms >
-
Member Resources for Funding Advantage & Individual Advantage
>
-
Agents
- Provider
- About Us
- Contact Us
Funding Advantage Explanation of Benefits
Your Explanation of Benefits (EOB) isn’t a bill. Instead, it gives you information about the amount your provider charged, the amount that will be covered by your benefit plan and any amount you might owe the provider. The EOB is mailed after your claim is settled. Your EOB also is posted on the Member Self-Service Site, which can be accessed on the home page.
How To Read Your Explanation of Benefits (EOB)
The sample is provided for informational purposes only. Key areas of an EOB:
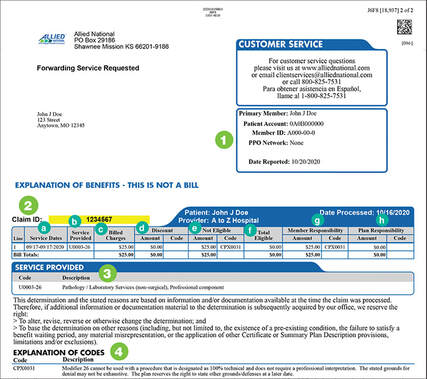
1. Member & patient information
2. Claim detail
4. Explanation of codes – Explanation of codes for discounts taken.
2. Claim detail
- Service Dates – The date each service was provided.
- Service Provided – A code that indicates what type of service was provided (the key can be found at #4 Explanation of Codes).
- Billed Charges – What your provider charged for the service.
- Discount Amount and Code – If the full cost of your service is not covered, the discounted amount and reason for the discount taken is given.
- Not Eligible – The dollar amount not covered by your plan.
- Total Eligible – The total expense that is eligible for benefits under your health plan.
- Member Responsibility – Your portion of the costs for service after the plan has paid benefits. You are only responsible for copays, deductibles, coinsurance and any services not covered by your plan. You ARE NOT required to pay the difference between what your provider billed and the discounted amount paid by Allied for these services. If the bill from your provider shows an amount due greater than your “member responsibility,” and you have paid your portion, contact Client Services at 800-825-7531.
- Plan Responsibility – The benefit amount payable by the plan for the service.
4. Explanation of codes – Explanation of codes for discounts taken.
IT'S VERY IMPORTANT that members alert us to these balance bill disputes immediately so that we can work with the provider to a resolution. In some cases, the provider doesn't contact us and immediately sends a balance bill which we do not see unless alerts by our members.
|
© 2022 Allied National, LLC. All Rights Reserved.
|
- Home
- Employers
-
Members
-
Member Resources for Funding Advantage & Individual Advantage
>
- Explanation of Benefits for Funding Advantage Members
- Member FAQs
- Member-Hybrid >
- Member-Traditional >
- Member-Essentials >
- Member-PPO >
- Member-Cost Saver >
- Member-Minimum Essential Coverage >
- Member - Community Health Plan >
- Member-H&H PLan >
- Member-Vault PPO Resources >
- Member-Vault RBP >
- Member-Fundamental Care
- Member-Fundamental Care Value Plan
- Member Resources for Individual Advantage
- Benefit Extras >
- Self-Service Login >
- Find A Provider
- Prescription Benefits
- Member Download Forms >
-
Member Resources for Funding Advantage & Individual Advantage
>
-
Agents
- Provider
- About Us
- Contact Us